Any links on this page that lead to products on Amazon and other companies may be affiliate links and we earn a commission if you make a qualifying purchase. Thanks in advance for your support!
Well, I have been on a strict 30 mg Lanzoprozole (proton pump inhibitor) regime for the last 5 weeks (together with 10 mg of amitriptylene daily) and I have to admit my acid reflux has been so much better.
Apart from occasional bouts of low grade heartburn, which has generally been sorted by a couple of tablespoons of Apple Cider Vinegar or gulps of Gaviscon Advance (recommended by my doctor), and sporadic sore throat / phlegm, I have been pretty much free of symptoms.
I visited my GP today, and she has reduced the dose to 15 mg of Lanzoprozole per day with a recommendation I continue to deal with any heartburn as I have been doing.
Night time reflux? Read how to avoid it here
Proton Pump Inhibitors
Whilst I am so relieved that this is the case, I’m back to worrying about the adverse effects of proton pump inhibitors.
Proton pump inhibitor (PPIs) have been on the market since the late 1980s and have replaced the histamine2 receptor-antagonists ( eg cimetidine, famotidine, nizatidine and ranitidine) as the most potent class of drugs for the treatment of acid-related diseases.
PPI’s rank as the 3rd highest selling drug class in the USA. Proton pump inhibitors were first introduced as a short term measure, but they are now often prescribed for years.
They are called ‘proton pump inhibitors’ because they work by blocking (inhibiting) a chemical system known as the ‘proton pump’. This chemical system is found in the cells in the stomach lining that make stomach acid.
Basically, this class of drugs stops the stomach producing acid, thereby reducing, if not eliminating, the symptoms of heartburn and acid reflux.
It does not, however, stop bile being refluxed, which is often a problem for some sufferers. It should also be borne in mind that PPI’s don’t work immediately – they can take up to 7 days to start having an effect on the symptoms.
However, despite the immense popularity of PPI’s, a recent survey by the American Gastroenterological Association, which covered more than 1000 individuals who took PPI’s to treat long term acid reflux or GERD (gastroesophageal reflux disease) found that more than 60% of the individuals continued to experience heartburn symptoms that disrupted their daily lives.
This may have something to do with how they are taken; A recent study, see ref 2, below, demonstrated that PPI’s were most effective when taken 1/2 hour before meals, and probably at their most effective when taken before breakfast.
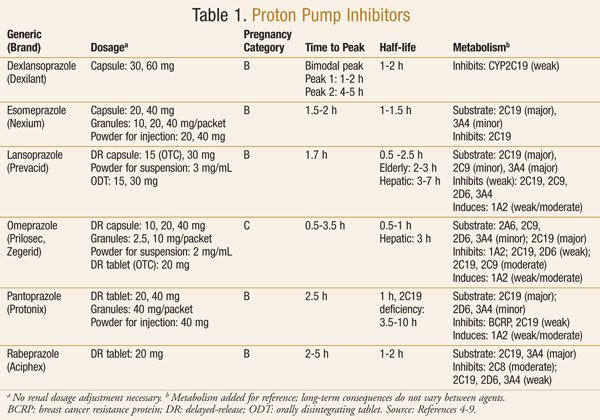
Types of PPI’s
PPI’s are generally available only on prescription, but you can buy omeprazole and pantoprazole over the counter at pharmacies in the US.
Below is a table taken from ref 1 (see at the bottom of the page) showing the PPI’s available at the end of 2013 (It provides more info than we need here, but it does show the key features of these drugs) :
Long Term Consequences of Proton Pump Inhibitor Use
Stomach acid is needed to absorb important vitamins and minerals, and a host of studies have related deficiencies in essential nutrients to increased long term PPI use, leading to the following issues:
- Increased risk of fractures
- Pneumonia and Clostridium difficile infections
- An 82% increased risk of all-cause mortality in those taking PPIs among the elderly (ref 3.)
- Elevated risk of heart issues
- Vitamin B12 and Magnesium deficiencies (see more here)
It is widely recommended to take supplemental B vitamins, particularly B12, and Magnesium, but do check with your physician to ensure these will not conflict with other medications.
The “Rebound Effect” of Proton Pump Inhibitors
As a result of these long term issues, many people (including myself) seek more natural alternatives to controlling acid reflux and heartburn, such as these here.
The Rebound Effect
The other notable issue with PPI use is that if you stop taking them, you could be subject to the “rebound effect”.
This is where the stomach cells go into overdrive and produce an excess of acid for a period of time until the body normalises. This is due to a surplus of the chemical gastrin, which is produced by stomach cells in response to a lack of acid (eg when you are taking PPI’s) – when the PPI’s are stopped, this excess gastrin signals the body to produce lots of acid.
To minimise the rebound effect, it is recommended to taper off the use of PPI’s over a short period of time, and to supplement this reduced use with H2 blockers, such as Zantac, and antacids, such as Gaviscon Advance, Tums and Rennies.
What have your experiences been with PPI’s? Please let us know in the comments below.
Leave a Reply